Release date: 2016-09-30
  IgorSpetic is the protagonist of this article and a volunteer for our research team at the Cleveland Veterans Medical Center. Now he is wearing a blindfold and noise-cancelling headphones and using his left hand to fumble out a bunch of cherries from the bowl in front of him. Is this a game? No, this is testing, because IgorSpetic's right hand has left him in an accident.

In the past few years, he has been using the myoelectric prosthesis developed by our team, and the real control of his "right hand" is the stretching of the muscles on the right arm. Traditionally, the decorative meaning of common prostheses for amputation patients is greater than the practical significance. In this test, the cherries taken with traditional prostheses are indeed very easy to be blasted.
Subsequently, we replaced him with a myoelectric prosthesis and activated a haptic system specially developed by the Functional Neural Interface Laboratory. Previously, our team of surgeons Anderson and Keith implanted electrodes in his right forearm and connected three major nerves through 20 contacts. In this way, Spetic can give a real feeling by stimulating different contacts on different nerves.
To test whether this "ghost hand"-like touch would allow Spetic to better control the prosthesis, we implanted a membrane pressure sensor into the device and used the model collected by the sensor to stimulate the nerve. As a result, the strength of the prosthetic cherries is much smaller, and Spetic smoothly picks up the cherry stalks.
In our series of tests, Spice successfully completed 93% of the tasks when the haptic system was turned on, but if the system was turned off, he would not even have a success rate when doing the task. In addition, according to Spetic, when he turned on the haptic system, he seemed to have a real hand, and the prosthesis was no longer a simple tool. Whenever we turn on the system, Spetic will say, "My right hand is back."
In the future, we hope to make the prosthesis as flexible as the human hand. However, our goal at the moment is to let Spetic forget that he has no right hand. Now, our haptic system is still in its infancy and can only be done in the lab. In the test, Spetic also needs to plug in various cables on the arm when completing the task, because we need to control the nerve stimulation through the computer. Even so, this haptic system is the first time ever to give a real feeling to an amputated patient. Right now, we are developing a system that can be fully implanted in the human body and hope to begin clinical trials within five years.
So how much can a prosthetic with a touch feel? As we all know, nowadays commercially available prostheses can only do some work that does not require precision, such as supporting the body balance. If a tactile system is added to the prosthesis, the confidence of the amputated patient in controlling the limbs will be greatly enhanced, and with the prosthesis, they will be able to complete some of the simpler tasks in the life of the car.
In addition to the uses mentioned above, we also hope that prosthetics can play a greater role in interpersonal relationships. Tactile sensation plays a big role in establishing the relationship between people. Without this ability, people will feel very lost. When we asked many amputated patients, they all expressed the hope that they could use their prosthesis to hold their lover's hand and feel the temperature of the other's palm. In the future, our technology will help them accomplish this dream.
I have worked hard for decades to solve the problem of the integration of humans and machinery. My extensive experience in biomedical engineering and neuroengineering has also kept me thinking about a seemingly simple question: How can I make electronic circuits and nervous systems accessible? If we find a solution, how do we transmit these sensory signals to amputated patients? In addition, in addition to liberating amputees, can this technology improve the quality of life of ordinary people?
In the past few decades, we have made great breakthroughs in this field, including the hardware that can be implanted into the human brain and body, and the ability to understand and simulate natural neural coding. In these codes, electron pulses in the nervous system can transmit information in brain cells and neurons throughout the body. These signals become the drive of the body, and the feedback they produce becomes the feeling of the amputated patient. In addition, the signal can also control the position of the limb and muscle strength.

Once the charge is implanted near the muscle or nerve, we can control the muscle contraction by sending a signal to control the charge. Recently, we are focusing on how to understand and repair the patient's sensitivity system.
In terms of the tactile perception interface, we mainly focus on connecting the broken limbs and the brain. However, the process is very difficult because we must strive for precision in terms of stimulation, and we must not damage or change the related nerves. For complete success, I am afraid it will take some time.
It's a bit easier to build an implant interface because we have a lot of options. The least harmful to the human body is the implantation of electric charge into the muscles near the nerves. This method has been widely used in the medical field, and it has a certain effect on spinal injury, stroke and other forms of nerve damage. In addition, under this method, the human body has a small reaction to charge rejection, and the charge replacement is also very simple. However, it requires a little more power when performing tasks, and sometimes it does not work well.
In addition to implanting the charge into the muscle, we can also place it near the nerve and the target axon, and here is the core area where the neuron handles the electronic pulse, which means that the amount of electricity required to complete the stimulation task is small, and we can have Selective stimulation of certain axons. However, it also has side effects, that is, the body will have a strong rejection of the charge, and sometimes it will directly discharge them out of the nerve.
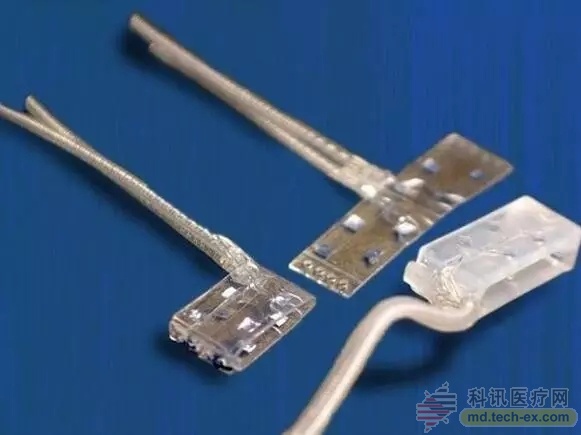
Restoring touch: In order to recapture the amputated patient, Case Western Reserve University researchers surgically implanted the charge into the patient's median, radial, and ulnar nerves. This time they used flat cuffs, this new product is more effective than traditional ring cuffs, because the electronic signal is more easily transmitted to the nerves. When a precise electronic pulse is introduced into the charge, the patient's palm and the specific part of the back of the hand will feel, and they can even feel different textures. Although this experimental system needs an external computer for the time being, R&D personnel will wirelessly control the controller in the future, so that the prosthesis can be easily controlled.
In both methods, a simpler muscle implant can only stimulate a point on a nerve, so it can be used for the treatment of epilepsy or to help stroke patients swallow and swallow. The more complicated axonal implantation method is mainly used to treat spinal injuries.
Since the late 1990s, our team has been developing such wraparound charges, which we call nerve cuffs. We have encountered many problems in the R&D center. How to interact with them without penetrating the nerves becomes one of the problems. The nerve contact surface is small and the traditional ring-shaped electric cuff cannot accomplish this task. Therefore, we flatten the nerve cuffs so that they can fully "close contact" with the nerves.
In 2014, we released the latest flat cuffs with 8 touch points built in, each of which is responsible for a stimulus. Now, this 8-channel cuff has been tested. The Spite we mentioned earlier implanted this cuff in the median nerve and ulnar nerve, but the other major neural nerve still uses the traditional Ring-shaped charge cuffs. With these devices installed, Spetic's forearm has 20 stimulation channels.
When Spetic first tested, we were completely unaware that the stimuli produced by the different channels differed in perception and orientation. We just nervously opened the device and activated a contact on his median nerve. "Wow," he screamed. "I have a feeling of thumb. This is the first time I have been injured!" At the same time, this moment also made our whole team feel happy.
After subsequent tests, we found that these 20 stimulating points actually allowed Spetic's "ghost hand" to react on 19 places, including the back of the hand, wrist and thumb.
Next, the contacts on our cuffs will increase to 4 times the current one. The increase in stimulation channels allows us to selectively connect more small axons so that the patient's feelings become richer. In addition to touch, we want to experience temperature, joint position, muscle intuition and even pain in the future. Although the word pain is somewhat sinister, it does have an important protective mechanism. In the test, a stimulation channel triggered a painful feeling.
Right now, we are continuing to develop new stimulation channels, and the system implanted in the Spetic body in May 2012 is still working well, and Spetic claims that when the system is turned off, he does not feel the presence of these charges.

From a technical point of view, it is one thing to trigger the patient's feelings, but how to control this feeling is another matter. The whole process is like talking, you need to make a sound, but if you want others to understand, you have to speak it out in words. In the first experiment, we made a mistake, causing Spetic to feel abnormal. At that time, we only sent out "sound" instead of "language."
In the second test, we replaced the electronic pulse mode and put the stimulus signal into the brain, but the test results are still not optimistic. Due to too many options, we still did not find the correct stimulus mode.
In order to speed up the test, I even started experimenting on myself. Because my hands are alive, the team members put a charge on my fingers, which can stimulate my superficial nerves. After the experiment started, we found that the intermittent change in pulse intensity made my fingers feel the pressure - just as someone was squeezing my fingers.
After testing successfully on my body, the team began testing on Spetic. He was a little confused when the stimulus started, but then he said he felt the pressure, just like putting his finger on the carotid artery. After fine-tuning, we changed a stimulating method, and Spetic felt a gentle touch this time, "just like someone puts a finger on my hand."
After research, we found that weaker pulses activate fewer neurons, while stronger pulses activate more neurons. In addition, the number of activated neurons is also controlled by the neural code in the brain. If our stimulation is synchronized with the neural coding, the patient can feel the touch.
With a simple neural coding, we are working hard to find more complex stimuli so that patients can get a more subtle touch. Right now, Spetic can already feel the texture of things. He can distinguish between velcro and sandpaper, and can feel the movement and shaking of objects. He can also feel the touch of others. Now, Spetic becomes more confident when using prosthetics.
Right now we are working with other labs to create an implantable stimulation system that can be completed with just a few artificial touch prostheses. The project is expected to be completed within 3 years and clinical testing will begin in 5 years.
It's not easy to build a complex nerve stimulation device that brings out the lab. The prosthesis needs to continuously monitor hundreds of tactile and positional sensors and pass the data back to the stimulator in real time, which is then translated into neural code for transmission to the nerve. At the same time, our system will also speculate on the user's intention by recording the exercise habits of the 16 muscles on the residual limb. These data will also be encoded and passed back to the body to generate stimulation signals to drive the prosthesis. Overall, the system will eventually have 96 stimulation channels and 16 recording channels. In addition, we will minimize the delay in stimulation.
In the process of system improvement, we tried to find the best value for the contact. If we use 3 flat charge cuffs (each with 32 contacts), we can create 96 contacts on the hand. So how many stimulation channels do we need? How can the information through these channels be adjusted and translated?
To create a stand-alone device that doesn't require an external computer, we need to implant a microprocessor in the prosthesis and let it shoulder the task of sending a stimulus to the charge cuff. In addition, these charges must also be durable and can work long hours in the human body.
This is definitely a daunting engineering challenge, but if we succeed, this haptic technology will affect the world. Not only amputated patients, ordinary people can also get a new touch, the doctor can directly feel the baby's heartbeat by hand, and the mine-clearing expert can touch the line to know which one to cut.
If all goes well, this vision will come true in the next decade. Feeling can help us distinguish each other. If we teach this ability to the machine, we can expand the scope of human control. Of course, the real desire of many people is actually very simple, that is, to feel the temperature of the palm of your lover again.
Source: Zhongguancun
Shrimp Frozen,Export Shrimp,Red Shrimp,Frozen Red Shrimp
Zhoushan City Shuangying Aquatic Products Co., Ltd.  , https://www.shuangying-aquatic.com